We arrived at Trailer Villa RV park on February 15, 2020, a Saturday. When I was setting up this assignment, Trailer Villa was the only RV park in a huge radius that had any openings for a long term spot. It was pricey! $2000/month plus electricity!
It sits overlooking a bay, but has no bay access. So, while we got a nice view, the water was not directly available to us. There are a lot of great areas to fish nearby and kayak though, so all good.

Trailer Villa RV park is clean and has a nice convenience store adjacent to the property for little items. We managed to get a nice pull through spot right across from one of the dog park areas. There was also a nice laundry room and shower house right there. We used the laundry room-still have to get the washing machine hoisted out to get repaired-but never did peak inside the shower house.

We got to park next to this sexy Newell diesel pusher. For those of you who aren’t part of the RV world, Newell and Prevost are THE motorhomes of all motorhomes. Some of these models can sell for over $2 million dollars. I love every inch of my Reva Mae and I could never be comfortable driving something that expensive (or even remotely afford it) but damn that was a beautiful rig to get to see close up. Even the headlights are sexy on that baby! I never got to meet the owners. Mike did. Guy said he was in town for some races and was from Oregon. Had a Tiffin at first, then got the Newell.
We had arrived on President’s Day weekend-an observed holiday for this company-so we had a few days to check out our new home area and get acclimated.

Bedwell Bayfront Park could be seen from our RV at Trailer Villa and was an easy walk or short drive to the entrance. This will be a great fall back place to hike with the dogs if I can’t get out. There are so many places in the Bay area I couldn’t wait to explore. Mike was born and raised in the east Bay-Fremont, but he knew little about this area so we were both excited to check out all it had to offer.

The park is 160 acres of trails that used to be a landfill. The landfill was closed in 1980 and now it is a park with a great trail system and a nature reserve. There are easy, flat hikes around the perimeter along with steep trails shooting off from the main loop. The views were fantastic. We had arrived toward the end of winter when the flowers are blooming and the grass is so green. We were both excited to see what this assignment and this location might bring!
Driving the other direction from the RV park, we found we were very close to the Redwood City Port. There were also nice walking trails along the harbor, a marina with the neatest ships, and a Google office. There was also a sailing school where young, eager beings learned to sail. Mike and I sat and watched a race one sunny afternoon. There were great places here the dogs could run and fetch and lots of walking.

Having done some weekend exploring and settling in, I started work at a facility in Mountain View, CA, just about 12 miles from the RV park on Tuesday.
The facility was experiencing some staffing issues, relying heavily on agency nurses and thus having some issues with documentation and carrying out orders. The team was young and hungry to get their facility up and running smoothly. It was going to be an exciting time but also fun!
My first week there, the DON who had 2 weeks left to work, called off for the entire week. She did come to work the second week and it was obvious while a kind person, she was in over her head and immensely overwhelmed. Floor staff were working doubles and insane overtime to cover vacancies and there were more resignations coming in due to the instability. The facility was in a vicious cycle that not even 2 agencies could help staff. We put out calls and got a third agency to help staff the facility.

After the DON left at the end of my second week, it was time to really get busy. If I was going to make an impact on this facility, I was going to have to put some hours in right off the bat.
Micah had been the Administrator for just a few months. He had worked his way up through the company starting in marketing and learning the ropes under the AIT program. This was his first building and his desire to not only succeed, but become a top facility was infectious and kept me going many days when I thought I could go no more. I will forever count him as a dear friend and I hope nothing but good things for him going forward. He is so deserving! With a wife and 4 children, I’m not sure the last time he has slept. Especially these days.

We quickly dove into the licensed nurse staffing issues. We contracted with a third agency to help lessen the burden and Micah looked at wages to ensure his rates were market compatible. We looked at shifts, the floor staff structure with the work flow, and then starting cleaning and tearing apart offices and nurse’s stations. (EVERY building I have EVER been in needed a thorough cleaning and organization of the nurse’s station and offices! Nurses are hoarders and can really be pigs-no offense. At one facility I found a dozen burritos in a bag that had been in the cupboard so long it no longer oozed or stank…true story) Quality staff deserve a quality area to work-and need to be held accountable to keep it that way-did I mention nurses are hoarders?
I penciled out a new hierarchy and work flow pattern for the floor and created a schedule that could be easily replicated (4/2) and allow consistent staffing on all the units. Micah and I also actively recruited and interviewed nurses, hiring the best candidates we could find. We were hiring 3-4 nurses each week and getting them started on the 2 week orientation process as quickly as we could.
Through this all, I was falling a little more in love with a small group of long term residents who hung together in the hallway I walked down several times a day. Raul, Glenda, and Ed became very special to me. They could break up the seriousness of my day as I walked by interacting with them. Glenda always gets her hair done in cute braids in different ways. Raul loves it when I “sing” his name like the old Yahoo commercials-“Raauuulllll” He loves to compliment me and tell me how beautiful I am. Ed enjoys a good joke and loves to make me feel appreciated. While I didn’t get a lot of time to bond with many residents, this trio was my family. They gave me the diversions I needed several times a day to get through the long hours rebuilding the facility structure.
I was still filling holes with recent resignations and barely limping by. In a nursing home, the Director of Staff Development is often the DON’s right hand-especially when there is no Assistant DON. Well our DSD had an urgent medical issue that took her out about 3-4 weeks into my assignment. Micah was a blessing. Stepping up to help with areas that he knew little about but learned quickly. It was highly stressful. But we were making progress. I was working long hours and trying to get multiple systems in place. Mike was minding the dogs and taking care of our home. He had been watching the news, while I was a bit oblivious to all that was starting to happen around me.
I had heard of the corona virus. I had seen blips of what was happening in Italy. But it was too late or I was too tired to watch the news after my long days. Like so many of you, it was so distant, I didn’t think much of it. I had worked during H1N1 scares, swine flu scares, you name it. This won’t be that much different, right?
Suddenly, I was getting little bits with dinner-they’ve cancelled an NHL Sharks game, the NBA is postponing games….at work, my officemate and case manager, Wen is updating me on things he’s read and seen about this “thing”. A random death with no underlying causes, New York is starting to blow up a little…..hmmm?!
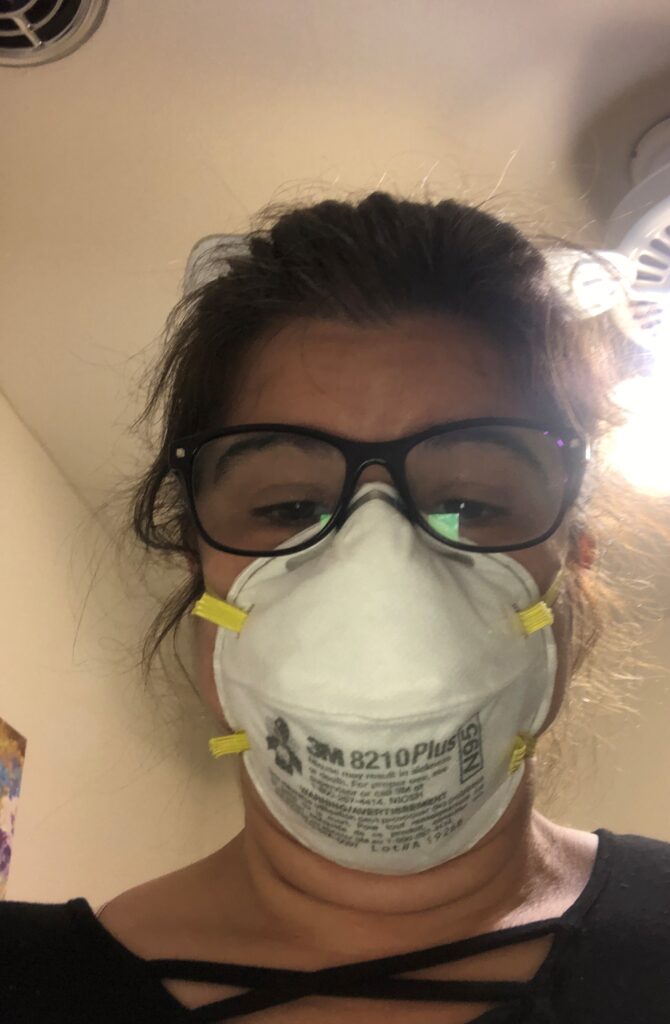
Wen and I start wearing masks-both of us has a bit of a cough-it’s full allergy season in the Bay area but maybe we should be cautious. We’re hearing more and more about PPE shortages-check inventory-NO N95 masks, well ok, other supplies are pretty good. This isn’t airborne anyway. Keep working on these systems, gotta fix this building yet!
At this point, staff are becoming more aware of the world around us as well. They want masks-we’re told no masks can be issued unless the staff has some type of symptoms-supplies are too short. We are reusing masks in paper bags for those that have allergy type symptoms. The panic is building.
One day we’re notified no visitors unless they are essential for the care of the resident-families who assist with feeding, home health aides, etc. We notify everyone and start screening.
Then just as soon we get that implemented, we’ve got daily calls with the county to update on PPE, cases, infection control practices, and the like. Next minute, the NBA has cancelled the season, we’ve been instructed to close and lock our doors to ALL visitors. What is going on? Can this be real?
Nursing homes are unique birds. Many residents have no visitors at all. Either they have no family, or they’ve been just left behind. But those that do have visitors, have fiercely dedicated visitors. Family that is involved, is usually ALL IN. Some come every meal to help encourage their loved one to eat. The dedication is amazing. Telling those family members they could not come back was so difficult. There were too many questions that could not be answered. When can I see mom again? How long will this go on? Who will feed her like I do? Can I just feed her? Please? One son was so distraught he told Micah to “call me when he dies.” He was certain his father would not eat without him being there every meal. Please keep them safe, please. We vowed to do our best to keep them safe from this invisible monster somehow. I will never forget the eyes and the looks and the fear and the panic. By this time the Seattle nursing home was on every newscast and the numbers dying was mounting both there and in New York.
I had one staff, an older aide-must have been in her 70’s. She wanted a mask. I asked her if she had symptoms-remember at this point we’re only allowed masks if we have symptoms-no, but you have to give me a mask. I can’t give you a mask unless you have symptoms. Trying to lead her, what are your symptoms? She was petrified. She said I saw on the news 3 people went to a concert, 2 did not have masks. The only one who lived had a mask. She told me I was killing her. I was just following orders and trying to preserve our supplies. (I gave her a mask. I couldn’t face the utter terror in her eyes and not give her a mask-if anyone asks, you have a cough!)
One night a local nursing home made the news. They had an outbreak-multiple cases. Another facility just down the street has a case. Santa Clara county now has the highest number of corona virus cases in California. I’ve brought my husband to the epicenter of the outbreak. We are a couple of weeks behind New York and body bags are piling up there. Oh, my dear God. This building is not staffed correctly yet, we’re using so much registry, I have to teach them so many things about infection control. There isn’t a DSD right now……okay buckle down. We can do this.
I’m responsible for all the residents in a 101 bed facility with about 68 long term, highly immunocompromised residents and 30 or so residents receiving short term rehab. That’s one of my faults. As a DON, I’m always responsible for everything. I believe that to my core and no amount of rationalization can remove that feeling from my very soul. If something happens, it is MY fault. Maybe that’s why I’ve been successful? Maybe it’s why I can only do this a few months at a time now. I don’t know. I just know it’s an important part of my fiber that I need to share if readers will get any idea of what my Covid 19 experience felt like to me. It’s not right or wrong or more or less, it just is…. It is my truth.
The Bay area shut down before California as a whole did. Going to the grocery store that last time was so surreal. Entire aisles were wiped clear. There were no eggs, no rice, no pasta, no flour, no sugar, no soups…..it was as if we had been dropped into an episode of The Walking Dead overnight. The sight alone was frightening.
98. I’ve got 98 residents to keep safe. 98. That was our census when this really started steam rolling through our lives.
We did so much training and educating and documenting on infection control over those first few days. Just as we thought we might have a minute to breathe, we received a call from an MD office. A patient who was in for a routine visit, the MD opted to test her for Corona Virus as a precaution, just wanted to let us know. We laughed a little and decided this would be good practice for infection control and isolation should a real scare ever come. We placed the patient on isolation and gave out all the training and education again on caring for this person.
March 21, 2020, we got the call. The patient had tested positive. Holy Crap! It was a Saturday. I met Micah at the facility and we got on the first of what seemed to be hundreds of corporate calls, family calls, staff calls and meetings. If we thought we had had long days up to that point, we were sadly mistaken. In a flash, 12-14 hours would have gone by. There was so much going on. A call from California Department of Public Health, a corporate call, a CDC directive, staff calling off….again.
With the help of the corporate office, we had put together what I thought was a great plan to announce that we had a positive patient, along with plans to care for that individual. Positive cases need to have dedicated care givers who do not interact with other staff or residents. If you recall, we were already challenged with staff and training new staff as quickly as we could.
When we announced to our staff, I knew there would be a certain level of panic and I knew already they would want masks. We got permission from corporate staff to give out surgical masks to those who wanted them. They’d have to reuse them, but we had to give them something. I knew several were close to walking out as it was, now with a positive case in house, we could not go in to this announcement without masks as an option, even if it wasn’t recommended by CDC then. In the end, I think this move may have saved some lives. Our staff were masking for the most part on March 21, weeks before it was recommended.
Because our positive patient had been asymptomatic and been in our facility for over a week prior to testing, walking all over and visiting with everyone, all staff and residents were considered to be potentially exposed. This designation allowed all staff to continue to mask and we masked all residents as well. We were screened and had temperatures taken twice daily. I really think this early potential exposure saved us. I still believe in masking in public places today.
We still lost several nurses and aides after the announcement. Even if they didn’t have to work with the infected resident, the thought, the potential for exposure was just too great for them. One young woman had JUST started. She was just off her orientation. It was her first job as a nurse. She lived with her parents and her grandparents. She had come to me several times prior, in tears. Her family had thought her risks, their risks were too high for her to work right now. Once they learned we had a positive resident, they forced her to quit. I understand, but it was still hard.
As a leader during this time, I think these were some of the hardest conversations to have with staff. We had to stay strong and help our staff stay strong. We could point out what we “knew” as truth regarding the virus. All the while, the news and the “truth” is changing faster than any of us can keep up.
This young lady would come to me and ask me if I was sure she would be safe. Yes, wash your hands and don’t touch your face. It’s not airborne-CDC says we’re all safe if we follow these practices. We have an obligation to our patients. You can do this. Educate your family and give them reassurances.
Another nurse had a one month old baby in her home. She never missed a shift. But she often had tears in her eyes, uncertain if she was doing the right thing, if she could really protect her family and work still. We had to be their rock, their voice of reason, all the while hearing the same uncertainties, they were hearing all day, every day.
Our day would be going somewhat smoothly, and then we’d get a call from CDPH or CDC or corporate or whomever, changing what we had just changed or implemented. Another news story of a healthy nurse or doctor dying. Another level of quarantine being implemented. How the fuck could I tell them yes, you’re safe? I know for certainty you are safe, when it changed every other minute? Doubt crept in often. I’m grateful for Micah and for Cindy, our rehab director. The 3 of us did our best to keep emotions hidden and keep the staff moving forward. We supported one another during the myriad of calls and changes and each had our points of breaking down. It was good to have people we could be people with-not just leaders.
A few tears and a few deep breaths and a refocus on what we could control. PPE supply was very short. We got 2 partial boxes of N95’s when we learned our patient was positive. Even with contingency use-reusing/storing/etc. -we were going to need supplies. As strong individuals, we could not sit back and just wait and rely on corporate to meet our needs. They had dozens of buildings to supply.
The county had set up systems to help get needed supplies to buildings and Micah worked on procuring as much as he could through those channels. Cindy and her supportive family found N95 mask overseas and ordered early. Groups making cloth masks popped overnight and we got on their lists for donations.
I began looking for possible alternatives. I found those silly tubular neck masks the fisherman use were plentiful and could be purchase relatively cheaply in bulk. We ordered 90 for our residents. It was something to protect them at least and conserved our medical masks for staff. Raul loved having a mask with a face on it!
We ordered disposable rain ponchos. We bought disposable kitchen aprons to use for residents who had infectious stool to preserve our small supply of disposable gowns for possible Covid cases-around this time it became Covid, no longer corona virus. Micah bought out Home Depot for painter’s overalls. We were really getting creative to keep supplies available to protect our staff.
Wen got the Chinese hook up started and through his wife was able to procure PPE from the Chinese community-so grateful for them.
Meanwhile, in house, we got our first few PUI cases. What is a PUI? Person Under Investigation. What that means is someone who had symptoms of potential Covid. When one of those cases developed, we had A LOT of work to do.
One resident who experienced a cough or a fever could put half a dozen residents on isolation. In the early days, if a resident developed a possible symptom, the roommates and anyone who shared a bathroom with that individual were all placed on isolation.
Once isolated, the county was notified of all the names of these residents, along with all the staff who worked with that resident when symptoms developed. Fortunately, Micah was able to get Teresa from another facility to help out as acting DSD. I would have drowned in paperwork and tears without Teresa. Thank you, Teresa for all of your help and support!
The county would send a nurse out to test the symptomatic PUI patient and we would receive results in 2-3 days. Meanwhile this resident and all of the roommates/bathroom sharers etc., would be required to stay on isolation and had to be cared for by dedicated staff-which could not include the dedicated staff caring for our Covid positive patient. More dedicated staff, more shifting around an already fragile staffing model. Digging and begging for staff.
I lost another nurse when I assigned him to the PUI cases. He wasn’t prepared for it. Probably my fault. I could have done better, but it was last minute and all I had. When he saw the assignment sheet, he walked out. He was petrified. He came back after a couple days off. He was remorseful and admitted he just wasn’t mentally prepared to work these cases. With our staffing issues we gladly took him back. Several days later he came to my office, visibly shaken. He was in the Reserves and had gotten orders. He was getting called up to work Covid. First thought was about karma. Then I looked at this beautiful, frightened human shaking in my office and the leader in me gave me all the pep talk I could muster. We’re medical professionals. Don’t think about what you can’t control. You need to think of what you can control. You can practice excellent infection control. You can take recommended vitamins and supplements. You can educate others. You can do this. You will be ok. It’s hard to see grown men so fearful. So unnerving.
I held my breath for each of those PUI cases. We had several over the next couple of weeks. We had to move patients, deep clean rooms, reassign staff, all the while we were still training and working with registry as we built the facility back up.
Each PUI sent my anxiety through the roof. Numbers were growing statewide. Santa Clara county was still number one-NOT a good number one. The news was inundated with Covid. Social media was inundated with Covid.
In the evening I was messaging with nurses I knew from all over-Iowa, SoCal, NorCal, sharing ideas and best practices and reconnecting with some I hadn’t heard from in years. I would come home, strip off my clothes, shower and then hold my husband and my dogs, often breaking down from the exhaustion of it.
I hated that. I didn’t want Mike to have to always hold me up. He was here, in this RV all day with no human contact, but the television that spouted Covid all day and night. I didn’t want to be one more thing on his mind. I didn’t want to be weak, for him, for my staff, for anyone. But damn, the tears came so easily.
I didn’t sleep much those days. I would have nightmares. I would research things we COULD do. I ordered a ton of plastic glad ware containers for better storage of our used N95’s one night after watching a video on FB. I would share ideas with fellow nurses all over. I would read AFL’s-those are All Facilities Letters-directives from the state health department and try to think of how we could meet the latest rules.
Eight days after our resident was confirmed positive, I wrote this on my FB feed,
Everything is moving so fast
Yet time is going so slow
And what I remember as normal
Seems so very, very long ago
Eight days. Most of everything I wrote, all 6 pages up to this point happened inside of those eight days. It was so very surreal. We, Micah, our team and I had lived what felt like months of experiences inside of eight damn days.
I remember those days, lying exhausted in bed and unable to sleep wishing I could just wake up from all of this. How can this be happening? Make it stop.
Each day felt like a week or more. So much was happening, there was so much to be done. So much new information and new directives to process. Each day was at least a week, but flew by in minutes. So surreal.
And through it all, more and more stories of healthy individuals coming down with the virus, healthcare workers dying, Santa Clara county numbers growing.
Maybe two weeks in we got somewhat numb. We had had multiple PUI cases and they were all negative. The county was giving new directives which reduced how much isolation a PUI and exposed roommates would receive-very conflicting data. They were also sending letters letting us know we could not refuse admissions for lack of testing. Funny, every resident we had to send to an essential MD appointment had to be tested prior to the appointment. However, I was not able to insist on testing for residents prior to admission to a nursing home full of highly susceptible elderly individuals? At one point, they sent a letter indicating we may be forced to take positive Covid cases.
Micah had been pretty rock strong through all of this, but this one nearly brought him to a breaking point. We sat in my office. He, Wen, and I and talked it out. I assured Micah we would NOT accept any Covid pts. We had worked too hard to protect Raul, Glenda, Ed and all the other long term residents to be forced to allow this deadly virus in our building. We were still caring for our positive patient and we hadn’t spread it, but it was tough and it was mentally exhausting knowing we were “sleeping with the enemy” every night and hoping we didn’t have one little slip of infection control that could kill most of our population.
Our facility was a union building-for all staff except nurses. I had already planned it out in my head when I saw the AFL indicating we may be forced to take Covid positive patients. I would grab the union aide rep, myself-who had nothing to lose-and one particular outspoken family member I had gotten quite close to and we would notify the media. I would NOT knowingly let this virus in without a fight. How dare they even think of using these people’s home to house infected people. I could not do that. I would not do that. Yet another thing to fear and prepare to battle against. Exhausting.
Meanwhile the media is talking about how easily this virus is spread and how long it lingers on surfaces, and more deadly cases among healthcare worker make the headlines. As I drive to work each day, I see the Home Depot parking lot packed. I pass landscape trucks and beer trucks, and read about people bitching that they can’t fish on social media. I see people breaking the shelter in place orders everywhere I look. I see them finding loopholes-fucking loopholes that may kill my patients. My anger is growing. I’m doing EVERYTHING I can, everything I can think of. This virus is a silent killer of the elderly. It could be anywhere and these people could be spreading it. One staff member makes one mistake at a gas station and I could lose my whole building. Who fucking cares about fishing you selfish pricks!? I’m living my truth at this point and I really don’t care about anyone else’s truth. I CANNOT lose these people. I cannot be a headline. I am not a villain. I love these people and I’m doing all I can.
It was somewhere around this time-a few more days in-maybe weeks-who knows-that we decided to offer groceries for our staff. I had people out searching for eggs, flour, etc. Every time they went to a store, our residents were endangered. We created sign up sheets and offered chicken breasts, eggs, flour, etc. to help our staff and keep them from going out. We preached every day to do all they could do to keep our little cocoon safe. Our residents were not to be feared, they were quarantined. It was the world outside that was a gross danger for them, and for us and our families.
Mike was so awesome. He understood the enormity of the task I had. He never complained. He often held me while I cried and went on and on about the landscapers and the beer trucks. He had opportunities to fish-safely-with friends. I knew he would be in his kayak and would be safe. He wouldn’t go. He knew there was always a chance he could bring it home and pass it to me and it could kill my patients. He stayed home and he supported me.
One day he went to the little convenience store, all masked up. As was normal practice, prior to going, he always asks if I need anything. My usual response is, “a diet coke” and ¾ of the time he forgets it. It’s our long standing joke. He, of course, forgot this time as well. Jokingly, I told him he’d better bring one to my funeral. Something I had said hundreds of times before as a joke, just hit wrong.
While remote, I knew there was somewhat of a chance Mike or I could contract this thing and end up as a headline-one of those rare cases that didn’t make it. I was working right down the hall from it 50-60 hours a week. I broke down…again.
Mike and I don’t pray. I’m agnostic and he is an atheist. We do believe in gratitude and the need to recognize it in our lives. So, each night at dinner we take a minute to reflect on our day and express our gratitude for all of our blessing. It’s like a prayer, but not, that I say every night at dinner. As we bowed our heads that night, my lips quivered and I tried so very hard to just breathe through it and speak and the words would not come out. My body wretched with silent sobs as I squeezed my eyes tighter trying to hold back the pain. I just couldn’t. Quietly Mike spoke, “we’d like to take a minute to reflect on our day….” It was a very powerful moment.
Quietly over the next few days, I made sure he knew where all the passwords and bank account information were located. Don’t get me wrong, I wasn’t petrified that I would die or he would die. I just needed him to know where things were….in case.
Our central supply manager had just lost her husband. She had driven him to the hospital for cardiac symptoms. She had to drop him at the door. She never saw him alive again. As I understand it, he contracted Covid while hospitalized with the cardiac condition and died. They had just gotten married in December. She buried him weeks later with a maximum of 10 attendees. She dropped him at the ED and never saw him alive again. This is America. How does this happen?
News was leaking out that wasn’t widely shared. Half of the entire Kaiser San Jose hospital was Covid positive. More nursing homes were being affected. Santa Clara county is still number 1. Will it ever end? What will our fate be? What will the fate of my residents be?
We had a nice lull for a minute. No new PUI cases. Staff were stabilizing. We had brought out blue tooth speakers and were playing music at the stations, trying to inject some fun, some levity to our situation. We worked hard during those weeks to finalize a master schedule and get systems stabilized. We were beginning to feel like old pros. Some of the directives coming out we had already implemented.
We had stopped all nebulizer treatments and changed to inhalers to reduce aerosol transmissions. We had taken it steps further and eliminated all the eye drops, inhalers, and nasal sprays we safely could stop or decrease. Anything to keep hands off faces. We were feeling pretty good.
Ed’s transport drivers came one day and as usual went through the screening process. One of them had a fever just over 100. Our system worked. The screener refused to let him past the desk and we notified all parties. We’re good. We’ve got this.
Until we received a call that Ed was being sent to the hospital from the dialysis center. He had become suddenly ill and they believed he had Covid pneumonia. My Ed? Not my Ed! I had done everything I could possibly think of to keep him and Glenda and Raul safe. I had failed. Please fight Ed. I’m so so sorry. I should have done more. I didn’t keep him safe. It was probably THE MOST painful, gut wrenching feeling as a nurse that I have ever had. I’m exhausted-mentally and physically. I’ve lost weight, I’m not sleeping well and my patient may have Covid despite all we did. Had we gotten lax? Where was the breach? He could have gotten it at the dialysis center. How can I keep my dialysis residents safe? Was Ed always masked when he visited at a social distance with Glenda and Raul? How many more? Who’s next?
We got the call a day or two later. Ed had died. We were still awaiting test results. I sat in my office and sobbed. Wen broke social distancing and hugged me. He knew I felt responsible for Ed. I was defeated. Everything we had worked for was to protect Ed and I failed. I wasn’t much of a leader that day.
As I drove home, I called my friend and coworker, Lisa who was a regional nurse with the company. I’ve no doubt I sounded like a huge mess. Lisa talked me down. She helped me refocus on what I could do and what an impossible task we nursing home staff were charged with trying to accomplish. How do you keep the ultra-vulnerable safe from a potentially invisible killer? Lisa was often my voice of reason. As a nurse she understood the challenges we faced and since she wasn’t on the front lines at that point, she could separate the emotions and craziness better. I’ll be forever grateful for her.
Of course, once I got home and Mike saw my face, the tears came again. I felt so very responsible for Ed. My whole, entire mission was to keep them safe. I had failed I had failed and Ed had died. Alone. He was all alone. My friend died alone. And it was my fault. Not really, but my heart could not let that go.
I received a text from one of my LVN’s that night, Rachelle, that helped me more than she will ever know. She had seen my tear stained face and felt compelled to reach out to me that evening. While I don’t have her exact words, she said something like I don’t know exactly what caused you to have so very much pain and I wish I could say something to take it away but when I saw your face today it confirmed what I already knew, how much you care and I thank you so much for that. Rachelle may never know how very much her words meant to me that night. The support of Mike and all the staff at the facility-Micah, Cindy, Susan who made me hot lemon tea with ginseng and lemon grass every day to stay safe, Wen, Cesar, Rachelle, Teresa-that’s what helped me get through this. They will forever be my family.
During the weeks the panic was growing, I thought often of leaving. Mike doesn’t have the best lungs. His sisters have both had cancer and he was a smoker for many years. We had started this life to LIVE. We had grandbabies to see. We had no debt. We didn’t need the money. We could be far away from everyone in the desert in a couple of hours and be free from all of this.
We both knew we couldn’t do that. I had made a commitment and I could not leave these people. Neither of us would be able to live with a choice to run. Even though I put him at risk every day that I worked. Just breathe, practice good infection control and keep going. That was all there was to do. With the focus from the media and nothing else on social media, this virus consumed every waking moment of our lives.
When I heard Ed had tested negative, I could not believe it! Post mortem tests were completed as well and he was negative. That extremely heavy weight was lifted. I didn’t have to live with this failure any longer. I had still lost a friend, who had died so sadly alone, but not because I could not keep him safe.
We used Ed’s death as a wake up call. We reinvested our efforts to practice and coach extreme, quality infection control. We could not be caught sleeping. We need to be ever diligent and aware of all the potential risks.
I turned 50 on April 10, 2020. It felt like it was months after our patient had tested positive for Covid but in reality, it was just a few weeks later. While we had planned a big party out of town, clamming and crabbing at the ocean, I spent it at work, hair graying, contact lenses put away for now-shouldn’t touch eyes, no make-up-gets the mask dirty. Not exactly how I had wanted to ring in the big 5-0.
The staff went out of their way to make my day special! We had cake, a surprise happy birthday serenade, and the rehab department gave me a fresh N95 mask. Susan, the Dietary Manager gave me eggs and some flour. It was one of the most special birthdays of my life. These simple things we take for granted so often were truly appreciated and I had genuine gratitude for the love around me that day.

The other “gift” we all received that day was that our patient who had tested positive for Covid and had been in our facility for just over a month, safely went home. We were no longer “sleeping with the enemy” Now all we had to do was keep our cocoon safe. One less huge risk factor gone. Great Birthday!
We had interviewed and hired a DON who was supposed to start just after my birthday. I would complete my assignment around April 22nd. We could see the light at the end of the tunnel and it looked like we ALL-my staff, my residents, and my husband-were going to get through this intact, alive, albeit a little more battle scarred.
The DON was a no-call, no-show. Who does that? Why? She made it through one week of off site orientation and never came back. She text her recruiter and said she didn’t think she could make a difference and only a nurse would understand. This was a highly educated-working on her doctorate-nurse in her late 50’s to early 60’s. Damn it, I am a nurse and I do not understand. She had us all snowed. I was certain she was going to provide the leadership this young team needed.
I agreed to stay on until May 1, 2020. Our site rental was up on the 1st, so we had a place to live until then, I might as well continue to work.
Through this 10 week nightmare, we had managed to hire and retain 14 nurses. We hired some of the most amazing young minds. We used our last agency nurse on April 11, 2020. As I completed the May schedule, there were no vacancies-and NO registry. We had a small on call nurse pool trained and ready. The building was cleaner than it had been in years, and we had kept Covid out.
My last day was so tough for me. I had met and loved so many wonderful people. We had gone through something together that only we could ever understand. I get it when old military men don’t talk about the war. You just can’t explain your truth to those who never experienced. It. Being with them all of those weeks, drawing strength from one another, was what got us all through it. While Mike knew A LOT, he could never know what we felt on those front lines.
We did not face what the ICU nurses faced. We did not face what New York City faced. It was different. It was not more. It was not less either. Each of us, throughout the world, have lived a different Covid truth these past few months. Some hardly affected at all, some profoundly affected.

Just before I left, someone left a beautiful orchid on my desk No one would confess. There was no card. Finally, as I was leaving and saying good bye to everyone, I learned where it had come from. Bea.
Bea is one of our older restorative aides. She’s a big, beautiful, warm woman who wears a white smock over her uniform every day. As I told her good bye and thanked her for everything, she became tearful. She hadn’t realized I was only interim staff. She said, I had hoped you’d be here forever. I just put the orchid on your desk to make it nice in there. I told her I had been trying to solve the orchid mystery for days and thanked her for it. She said, all these years, you were the first to really care about us. No one had asked me how I was doing every day like you do. Wow. Thank you, Bea. I will miss you.
I am so proud of the team I survived Covid alongside. This is one of the finest groups of people I have ever met. I love all of you and wish you all of the best as you continue to navigate these dark waters. While I may never speak or see some of you again, you will always be a part of what makes up me.
My fear is that media will not shine fairly on nursing homes. We, the staff who care for the old and forgotten, are not villains. We are doing the very best we can in a very uncertain and unstable world. We have not been given a fair chance with this invisible virus. Our patient had no symptoms. Had she not been tested; she could have taken out our whole population without even realizing it. We got lucky she happened to be tested. We are the last to get PPE. We are not able to request testing prior to admitting a patient. We are receiving patients with questionable test results. We live knowing every day the outside world is not taking the precautions we so desperately need them to take so that we can get safely to and from work every day and avoid infecting our residents. I’m not sure what the world expects of nursing homes but the staff are doing all they can to ensure safety. Please show them the same gratitude you’re showing the hospitals and other medical settings. Our patients are the MOST vulnerable.
There is so much more. So many little moments that are burnt into my soul that only a very few could ever understand. I guess I have a little case of PTSD. This journey will not define me, but it will forever be part of me. It has changed me. There are moments of reflection and tears still to this day. I am grateful for it. I think I have a higher level of compassion and a truer sense of what is really important to me. I am grateful for the people who came into my life and my heart through this. And I’m grateful my tour of duty has been completed. I check in often and keep this team close to my heart. They are strong and still Covid free. May they get through this stronger and better than ever. May we all.


Patty: this was utterly amazing ! I truly felt touched and could not stop reading. It broke my heart yet gave me strength. Thank you for sharing this with us. You are truly an angel that was meant to be a nurse! Take care and enjoy now. Jane’e
Thank you! I’m so glad you “got” my feelings in this. It was tough to write it. I cried a lot but so therapeutic. I feel like I can move in now. Thank you for your kind words!
Oh my god Patty you’re making me cry! If you would have let me strap my Prius to Reva Mae, I could’ve been your DSD! Haha. But seriously, you are an amazing nurse and a great mentor. In the short time I’ve known you, you have really inspired me to be a better nurse. You have always been absolutely kind and compassionate towards the residents and staff. You have managed to eloquently express the fear, dread, anger, and uncertainty us healthcare workers (and all
other essential workers) feel. Thank you and we miss you!
I would have loved to have worked with you again! Thank you for such kind words Miss Meghan! I miss you guys so much! I’m excited knowing I’ll be in my SD home this winter. Definitely more hikes and more fun to come! We have got to go back to Mexico too!
You’re a wonderful writer. I felt like I was right there alongside you while I read it. Its frustrating when people try to make the people working in SNFs out to be villains when they are stuck in a very hard place and many are doing their best. You’re a great nurse and leader, Patti. Enjoy your time decompressing from it all.
Thank you Chelsea! I have loved watching you grow from cna,lvn, Rn, wife. Can’t wait to see what you do next! You’re pretty darn amazing!